arkansas total care prior authorization
Communicate to all personnel involved in outpatient scheduling that prior authorization is required for the above procedures under Arkansas Total Care. 02400249 All-inclusive ancillary psychiatric 0901 09050907 0913 0917 Behavioral health treatment service 09440945 Other therapeutic services 0961 Psychiatric professional fees Forms.
Authorization requests may be submitted by fax phone or secure web portal and should include all necessary clinical information.

. Prior Authorizations for Musculoskeletal Procedures should be verified by TurningPoint. Account Manager Secure Portal PDF PAI Provider Self Reporting Form PDF. Prior Authorization Processes To ensure that authorization numbers have been obtained the following processes should be considered.
Monday through Friday with the exception of holidays. If an authorization is needed you can access our login to submit online. Arkansas Health Wellness providers are contractually prohibited from holding any member financially liable for any service administratively denied by Arkansas Health Wellness for the failure of the provider to obtain timely authorization.
1-833-249-2342 Standard requests - Determination within 5 calendar days of receipt of request. CPT codes that require prior authorization by AFMC can be found in your. Urgent Requests - Determination within 1 business day of receipt of all information necessary to complete request.
Along with this form the medical professional should include any relevant clinical documentation that supports their justification to request. Physicians will be able to begin submitting requests to turningpoint for prior authorization beginning on 12162019 for dates of service on or after 112020. Sign into your Secure Provider Portal Once inside the.
NIA can accept multiple requests during one phone call. Should you have any questions at this time please contact the Arkansas Health Wellness Health Plans Provider Services Line at 800 294-3557. Use our tool to see if a pre-authorization is needed.
There is no limit for children younger than 21. An Arkansas Medicaid prior authorization form must be filled out and submitted to Arkansas Medicaid in order for medical offices to request State coverage for a non-preferred drug prescription. Any anesthesiology pathology radiology or hospitalist services related.
Submitting an Authorization Request The fastest and most efficient way to request an authorization is through our secure Provider Portal however you may also request an authorization via fax or phone emergent or urgent authorizations only. You should always use our websites authorization page to determine whether a procedure code requires prior authorization and always check eligibility and confirm benefits before rendering Behavioral Health services to members. The following information is generally required for all authorizations.
Its quick and easy. Existing Authorization Units For Standard requests complete this form and FAX to 1-833-526-7172. To request authorization call AFMC at 800-426-2234 between 830 am-12 pm.
You further agree that BAAA and its affiliates its directors officers employees and. Visit the Arkansas Total Care Home Page Click on For Providers on the home page. 81220 Informational webinars are.
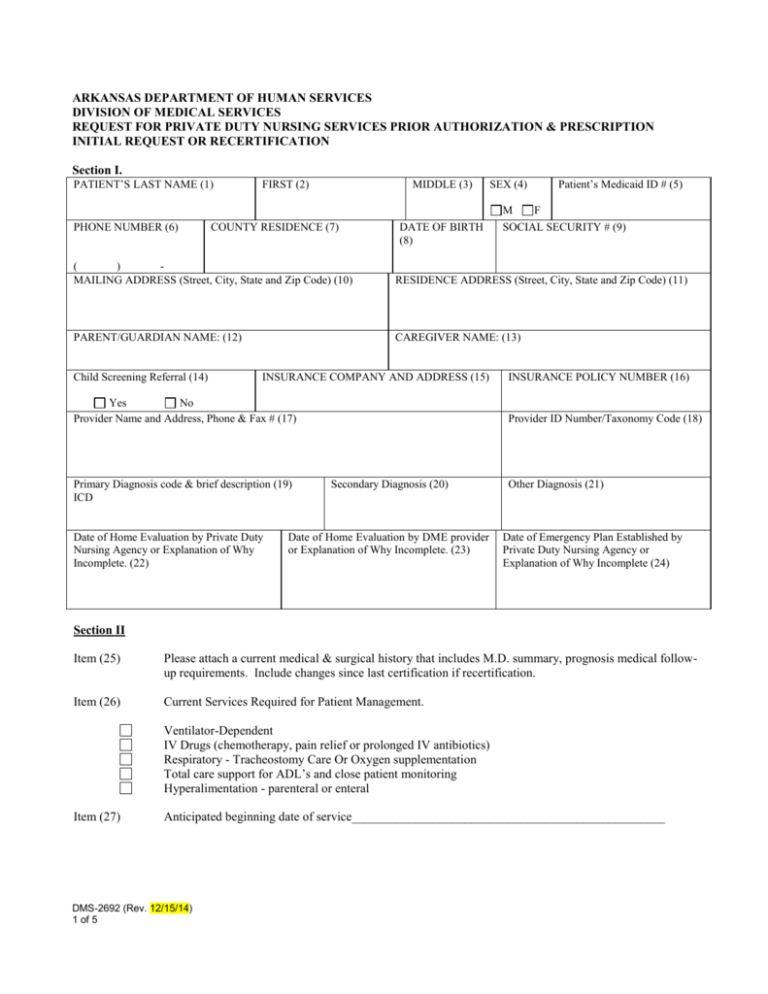
For adults age 21 and older Medicaid will pay for a limited number of days of inpatient hospital care. DMS Medical Assistance Dental Disposition DMS-2635 Gainwell Technologies Financial Unit Stop Payment Affidavit Office of Long Term Care Forms Prescription Drug Prior Authorization Forms. Pre-Auth Check Tool - Ambetter.
Failure to do so may result in denial of reimbursement. Prior Auth Change Update PDF Check to see if a pre-authorization is necessary by using our online tool. Arkansas total care prior authorization Friday March 11 2022 Edit.
Sincerely Arkansas Health Wellness Turning Point Prior Authorization Training Date. You will have to pay a co-pay if you are 18 or older or have ARKids First-B. HOW TO SUBMIT A PRIOR AUTHORIZATION Follow the steps below to submit a Prior Authorization PA 1 STEP 1.
All inpatient admissions require prior authorization. You may obtain a prior authorization by calling 1-866-500-7685. 833-249-2342 Standard Requests - Determination within 2 business days of receipt of all information necessary to complete request.
Prior authorization requirements are subject to periodic changes. Services billed with the following revenue codes always require prior authorization. Urgent requests - I certify this request is urgent and medically necessary to treat an injury illness or condition not life threatening within 72 hours to avoid complications and unnecessary suffering or severe pain.
2 A candidate must have sufficient motor skills to gain access to clients in a variety of care settings and to manipulate the equipment central to the treatment of patients receiving anesthesia. The hospital might need to get Medicaids approval first. Member name Member ID number.
Others are added as they become available. 711 3 STEP 3. Determination made as expeditiously as the enrollees health condition requires but no later than 14 calendar days after receipt of request.
To determine if a specific outpatient service requires prior authorization utilize the Pre-Auth Needed tool below by answering a series of questions regarding the Type of Service and then entering a specific CPT code. Telephone Access Call center hours of operation are Monday through Friday 8 am. The program will include the following Arkansas Total Care Membership.
Access eligibility and benefits information on the Availity Portal or call Provider Services at 1-844-462-0022. To determine coverage of a particular service or procedure for a specific member. INPATIENT MEDICAID PRIOR AUTHORIZATION FORM Complete and Fax to.
While it is the responsibility of the rendering physician to obtain prior authorization facility providers are encouraged to contact TurningPoint to verify the prior authorization has been completed for Arkansas Total Care members prior to admission. Arkansas Total Care Prior Authorization. Those requests must be processed by calling 1-866-500-7685.
See Procedure for Obtaining Prior Authorization in the Arkansas Medicaid Provider Manual Section 262000 page II-77. Verify benefit coverage prior to rendering services. Updated December 31 2021.
Arkansas Health Wellness Manuals Forms. For Expedited requestsplease CALL 1. Medicaid and ARKids First will pay for hospital care that is needed for your health.
Use the Prior Authorization tool above or within the Availity Portal. Some of the forms used by Arkansas Medicaid and its providers are available in electronic format. If a physician office calls to schedule a patient for a procedure.

Frequently Asked Questions For Providers Arkansas Department Of Human Services